About Benetti Foundation
Benetti Foundation
Articles by Benetti Foundation
Surgical Implantation of Stem Cells in Heart Failure Patients due to Idiophatic Cardiomyopathy
Published on: 25th July, 2017
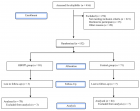
OCLC Number/Unique Identifier: 7317595690
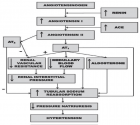
Introduction: Congestive heart failure is one of the main causes of morbidity and mortality in the XXI century given the promising to date of ABMDSCs and HFDSCs we investigate the safety and efficacy for the implantation of those stem cells for the treatment of idiopathic cardiomyopathy. This is the first pilot clinical study to assess the safety and feasibility of HFDSC in humans. We totally implanted 13 patients: 3 patients were implanted with ABMDSC by Mini-invasive surgical technique in March 2004 in Montevideo, Uruguay, and 10 patients were implanted with HFDSCs by using 2 different surgical techniques: minimally invasive technique (1 patient) and full sternotomy technique (9 patients) between January and February of 2005 in Guayaquil Ecuador.
The HFDSCs were obtained from fetuses of 5 to 12 weeks´ gestation from legally consent, no compensated donors who have undergone terminated ectopic pregnancies, elective abortions, or spontaneous miscarriages. At that gestation´s period, totipotent stem cells´ fetus haven´t develop yet the HLA histocompatibility complex, so there´s no possible antigenicity between donor and recipient.
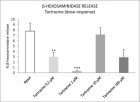
Results: Patients with HFDSCs improved in association with increased contractility in these regions. Compared with baseline assessments, we noted other improvements: The mean (±SD) NYHA class decreased from 3.4±0.5 to 1.33±0.5 (P=.001); the mean EF increased 31%, from 26.6% ± 4.0% to 34.8%±7.2% (P=.005); performance in the ETT increased 291.3%, from 4.25 minutes to 16.63 minutes (128.9% in metabolic equivalents, 2.45 to 5.63) (P<.0001); the mean LVEDD decreased 15%, from 6.85±0.6cm to 5.80±0.58cm (P<.001); mean performance in the 6-minute walk test increased 43.2%, from 251±113.1 seconds to 360±0 seconds (P=.01); the mean distance increased 64.4%, from 284.4±144.9m to 468.2±89.8m (P=.004); and the mean result in the Minnesota congestive HF test decreased from 71±27.3 to 6±5.9 (P<.001) The Kaplan-Maier probability of survival at 48 months was 66%.
It is not observed rejection, these patients have not developed malignance nodules or cancer at all in the follow-up. In the AMBCSs. The preoperative average NYHA functional class was 3.4; at. 6 months of follow up the average functional class value was 1.3 (p<0,005);. After 6 months all of them remained in functional class I/II. Baseline values of LVEF were 25,28 and 30%.; at 6 months increased to 38, 40 and 46%. (p<0,05). LVESV went from 50mm to 42mm (p<0.05). After 24 months, 2 of the patients still maintained this improvement, while the 3er patient returned to the earlier values after suffering from pneumonia. At 12 years and 5 months 2 patients are alive both received a Resynchronization Therapy; at 8 years and 3 months and 9 years and 1,6 month the actual average EF are 28 and 30 %. The 3er patient died of sudden death at 10 years after the implantation. We can´t demonstrate the cause of this sudden death.
Conclusion: Irrespective of the improvement seen in this study, it is still premature to determine accurately the mechanism of action, indications, doses and type of stem cells. Therefore, is imperative and extremely important that more research is needed.
Stem cells in heart failure some considerations
Published on: 25th January, 2018
OCLC Number/Unique Identifier: 7325111402
Stem cell treatments depend not only on the type of cell to be used but also on the different implantation techniques. Intravascular cell injections are known to rapidly separate from the vessels. On the other hand, it is also well known that direct injection into the myocardium provides better coupling within the heart muscle. That were the cases of Embriofetal stem cell (HFDSC) or Autologous stem cells (ABMSC) in our experience focused on direct approaches.
Stem cells in patients with heart failure experience
Published on: 20th April, 2018
OCLC Number/Unique Identifier: 7666352115
Between 2003 and 2011, 17 patients with heart failure were treated with stem cells as part of our Foundation’s Regenerative Medicine program. In several centers and countries 4 with ischemic cardiomyopathy of which 3 were surgically implanted with autologous bone marrow stem cells (ABMSC) plus bypass surgery. One patient was treated with hyperbaric medicine plus bypass surgery. Patients with idiopathic cardiomyopathy were implanted surgically with 2 different types of stem cells. Ten patients were implanted with stem cells derived from human fetuses (HFDSCs) and three patients with autologous bone marrow stem cells (ABMSC). The ejection fractions of the coronary artery bypass graft off pump OPCAB (control group) versus coronary artery bypass group off pump OPCAB plus stem cell transplantation were as followsin the entire serie: preoperative, 30.7% +/- 2.5% compared to 29.4% +/- 3.6%; 1 month, 36.4% +/- 2.6% versus 42.1% +/- 3.5%; 3 months, 36.5% +/- 3.0% vs. 45.5% +/- 2.2%; And 6 months, 37.2% +/- 3.4% versus 46.1% +/- 1.9% (p <0.001). The first patient performed at our center in Argentina in this series is alive and asymptomatic 15 years after implantation, and the rest of this series we do not have current data. A patient without visible vessels in the anterior wall of the left ventricle was treated with 18 hyperbaric chamber sections from one hour at 1.4 AT. After creating angiogenesis, the patient was operated on receiving 2 grafts (mammary and venous) without extracorporeal circulation in the anterior descending artery and diagonal artery. The preoperative ejection fraction was 33% at 90 months of follow up the ejection fraction was 58%. The patient at 90 months was asymptomatic. Of the idiopathic heart disease group, nine patients underwent median sternotomy, and received human fetal stem cells (HFDSCs from ectopic pregnancy or spontaneous abortion, three patients received autologous bone marrow stem cells ABMSC) and 1HFDSCs for Minimally Invasive Surgery.
Patients with HFDSC, compared to baseline, improved: The mean (±SD) NYHA class decreased from 3.4 ± 0.5 to 1.33 ± 0.5 (P = 0.001); Mean EF increased 31%, from 26.6% ± 4.0% to 34.8% ± 7.2% (p = 0.005); the yield in ETT increased 291.3%, from 4.25 minutes to 16.63 minutes (128.9% in metabolic equivalents, 2.45 to 5.63) (P <0.0001); the mean LVEDD decreased 15%, from 6.85 ± 0.6cm to 5.80 ± 0.58cm (P <0.001); the mean performance on the 6-minute walk test increased 43.2%, from 251 ± 113.1 seconds to 360 ± 0 seconds (P = 0.01); the mean distance increased 64.4%, from 284.4 ± 144.9m to 468.2 ± 89.8m (P = 0.004); and the mean score in the Minnesota congestive HF test decreased from 71 ± 27.3 to 6 ± 5.9 (p <0.001). Kaplan-Maier’s probability of survival at 40 months was 66%. No rejection or cancer was observed at follow-up, in this series follow-up was discontinued at 4 years. In idiopathic patients receiving autologous cells by Mininvasive technique preoperative NYHA was 3.6 (+/- 0.70) 6 months after receiving stem cell therapy. The mean value of the functional class was 1.9 (+/- 0.90) (p <0.005). ) showing marked clinical improvement. The preimplantation ejection fraction was 28% (+/- 3.6%) and at 6 months 44% (+/- 4.7%) (p <0.005). There was a similar change in ventricular diameters: After 6 months LVESV went from 50mm (+/- 3.3) to 42mm (+/- 4.5) (p <0.05). Two of the three patients in this group received re-synchronization therapy; one died at 10 years and 4 months, another at age 11 and another one alive at 12 years of the implant. More experience should be performed with different techniques and cells to find the appropriate treatment in this type of patients.

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."